During the past two weeks of my clinical rotation at Mon General Hospital, I have been employing the Nutrition Care Process whenever I am consulted on a patient. The Nutrition Care Process (NCP) is a systematic approach used in clinical dietetics in order to provide the best care for the patient. The NCP provides a framework for the RD to assess each patient’s individual nutritional needs and interventions. There are four steps to the Nutrition Care Process:
1) The Nutrition Assessment – “A systematic process of obtaining, verifying, and interpreting data in order to make decisions about the nature and cause of nutrition-related problems”. In the nutrition assessment, the RD should obtain as much information about the patients anthropometric data, medical history, diet history, current diagnosis, medications, lifestyle, etc.
Example of data to collect from a patients medical chart:
- Ht, Wt, BMI, Ideal BW, Usual BW, % Ideal BW
- Current diagnosis and current condition
- Medications and possible food-drug interactions
- Family medical history, past surgeries
- Current diet at the hospital
- Meal intake %
- Assistance with meals?
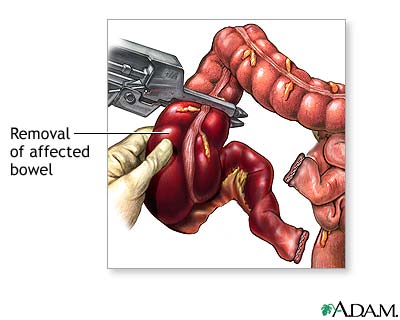
- Bowel movements and bowel sounds
- Functioning of the patient’s GI tract
Examples of questions to ask the patient during the initial assessment:
- Typical diet or any special diet at home
- Have you ever been instructed on any special diet before?
- Food allergies/dislikes/intolerances
- Usual body weight or any weight changes in the last year?
- Do you cook or eat out? Live alone or with anyone?
- 24-hr recall
- Food frequency questionnaire
- Swallowing/chewing difficulties
- Drink alcohol or smoke?
- Typical physical activity and how much
- Vitamin, nutritional, herbal supplements?
- Why typically shops for groceries?
- Do you read food labels?
Determine patient’s nutritional needs:
- Based on the person’s current diagnosis and condition, determine their energy needs using the appropriate equation recommended by the Academy of Nutrition and Dietetics Nutrition Care Manual (ex: kcal/kg, Mifflin-St. Jeor, Ireton-Jones, etc).
- Determine protein, fluid, and any other nutrient needs that are pertinent to the patient.
2) Diagnosis – This is a nutritional problem that the dietitian is responsible for diagnosing and treating. A formal nutritional diagnosis consists of three components: Problem “related to” Etiology “as evidenced by” Signs/Symptoms. (Or PES Statement for short).
- Problem: A nutritional problem is broken down into 5 different domains, each with several subtopics. The 5 domains are calorie energy balance, oral or nutrition support intake, fluid intake balance, bioactive substances balance, and nutrient balance.
- Etiology: The etiology is the cause or contributing factors related to the problem.
- Signs/Symptoms: These are defining characteristics that provide evidence that the problem exists. These characteristics are usually measurable or quantifiable.
Example PES statement: Excessive calorie intake (P) related to regular consumption of large portions of high-fat meals as evidenced by diet history & 12 lb wt gain over last 18 mo (S).
Example PES statement: Altered GI function (P) R/T ileal resection (E) as evidenced by medical history and dumping syndrome symptoms after meals (S).
3) Intervention – “Purposely-planned actions designed with the intent of changing a nutrition-related behavior, risk factor, environmental condition, or aspect of health status for an individual, a target group, or population at large”. The nutritional intervention should be quantifiable and obtainable by the patient. The intervention could include a change of diet (tube feeding or TPN), nutrition education and counseling,increasing the frequency/types of food choices, etc.
Example of Nutritional Intervention: Pt will include at least one nutrient-dense supplement per day in his diet.
Example of Nutritional intervention: Pt will increase energy intake to 1800 kcal per day, complete 3-day food record for analysis of adequacy.
4) Monitoring/Evaluation-The monitoring and evaluation step is meant to determine if the RD’s intervention had a positive outcome on the patient. Monitoring in an in-patient setting could be anywhere from 3-5 days.